Diabetes mellitus is defined as a collection of metabolic diseases characterized by high blood sugar (glucose) levels that result from defects in insulin secretion, or its action. Diabetes was first recognized as an ailment connected with "sweet urine," and extreme muscle loss in the olden world. High levels of blood glucose (hyperglycemia) lead to spillage of glucose into the urine, therefore the term sweet urine
Type 1 Diabetes symptoms
Symptoms of diabetes
can be associated in type 1 diabetes, which is usually diagnosed in children
and teens, and type 2 diabetes, which most frequently occurs in adults. The
symptoms of any of the two types are connected to high blood and urine glucose
levels and include :
- Frequent infections
- Nausea
- Vomiting
- Blurred vision
- Hunger
- Dehydration
- Weight loss or gain
- Fatigue
- Dry mouth
- Slow-healing wounds, cuts, or sores
- Itching skin and
- Increased susceptibility to infest
The symptoms of type 2 diabetes includes :
- Increased urine output
- Excessive thirst
- Weight loss
- Hunger
- Fatigue
- Skin problems
- Slow healing wounds
- Yeast infections and
- Tingling or numbness in the feet or toes.
- The early symptoms of untreated diabetes are related to elevated blood sugar levels, and loss of glucose in the urine. High amounts of glucose in the urine can cause increased urine output (frequent urination) and lead to dehydration.
- The dehydration also causes increased thirst and water consumption.
- A relative or absolute insulin deficiency eventually leads to weight loss.
- The weight loss of diabetes occurs despite an increase in appetite.
Some untreated
diabetes patients also complain of fatigue.
Nausea and vomiting can also occur in patients with untreated diabetes.
- Frequent infections (such as infections of the bladder, skin, and vaginal areas) are more likely to occur in people with untreated or poorly-controlled diabetes.
- Fluctuations in blood glucose levels can lead to blurred vision.
- Extremely elevated glucose levels can lead to lethargy.
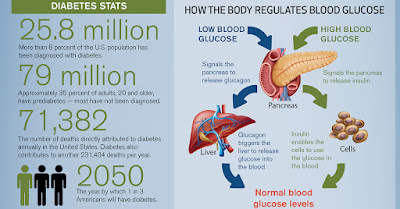
Insufficient
production of insulin (either completely or relative to the body's needs),
production of faulty insulin (which is unusual), or the incapability of cells
to use insulin correctly and efficiently leads to hyperglycemia and diabetes.
- This latter state affects mostly the cells of muscle and fat tissues, and results in a condition known as insulin resistance. This is the chief dilemma in type 2 diabetes.
- The complete lack of insulin, usually secondary to a critical procedure touching the insulin-producing beta cells in the pancreas, is the main chaos in type 1 diabetes.
In type 2 diabetes,
there also is a stable reject of beta cells that adds to the procedure of
elevated blood sugars. Basically, if somebody is resistant to insulin, the body
can, to some quantity, boost production of insulin and conquer the level of
resistance. After time, if production decreases and insulin cannot be released
as dynamically, hyperglycemia develops.
There are two major types of diabetes, called type 1 and type 2.
Type 1 diabetes was also previously called insulin dependent diabetes mellitus
(IDDM), or juvenile-onset diabetes mellitus. In type 1 diabetes, the pancreas
undergoes an autoimmune assault by the body itself, and is rendered powerless
of building insulin. Unusual antibodies have been found in the majority of
patients with type 1 diabetes. Antibodies are proteins in the blood that are component
of the body's immune structure. The patient with type 1 diabetes must rely on
insulin medication for endurance.
In autoimmune diseases, such as type 1 diabetes, the immune structure
erroneously manufactures antibodies and inflammatory cells that are directed
against and cause injure to patients' own body tissues. In persons with type 1
diabetes, the beta cells of the pancreas, which are accountable for insulin
production, are attacked by the misdirected immune system. It is supposed that
the predisposition to develop abnormal antibodies in type 1 diabetes is, in
part, hereditarily inherited, although the facts are not fully understood.
Exposure
to certain viral infections (mumps and Coxsackie viruses) or other
environmental toxins may serve to trigger abnormal antibody responses that
cause injury to the pancreas cells where insulin is made. several of the
antibodies seen in type 1 diabetes include anti-islet cell antibodies,
anti-insulin antibodies and anti-glutamic decarboxylase antibodies. These
antibodies can be detected in the majority of patients, and may help determine
which individuals are at risk for developing type 1 diabetes.
Type 1 diabetes tends to happen
in youthful, lean individuals, generally before 30 years of age; though, older
patients do present with this form of diabetes on occasion. This subgroup is
referred to as dormant autoimmune diabetes in adults (LADA). LADA is a slow,
progressive form of type 1 diabetes. Of all the people with diabetes, merely about
10% have type 1 diabetes and the remaining 90% have type 2 diabetes.
Type
2 diabetes was also formerly referred to as non-insulin dependent diabetes
mellitus (NIDDM), or adult-onset diabetes mellitus (AODM). In type 2 diabetes,
patients can still manufacture insulin, but do so relatively poorly for their
body's needs, predominantly in the face of insulin resistance. In several cases
this actually means the pancreas produces bigger than normal quantities of
insulin. A major feature of type 2 diabetes is a lack of sensitivity to insulin
by the cells of the body.
In addition to the tribulations
with an increase in insulin resistance,
the release of insulin by the pancreas may also be imperfect and suboptimal. In
fact, there is a recognized stable decline in beta cell production of insulin
in type 2 diabetes that contributes to worsening glucose control. (This is a main
issue for several patients with type 2 diabetes who eventually require insulin
therapy.) lastly, the liver in these
patients continues to produce glucose through a process called gluconeogenesis regardless
of elevated glucose levels. The control of gluconeogenesis becomes compromised.
While it is said that type 2 diabetes occurs frequently in persons over 30 years old and the occurrence increases with age, an alarming number of patients with type 2 diabetes are scarcely in their teen years. The majority of these cases are a straight consequence of deprived eating habits, higher body weight, and lack of exercise.
While there is a strong
genetic component to developing this form of diabetes, there are other risk
factors - the most significant of which is obesity. There is a
direct relationship between the degree of obesity and the risk of developing
type 2 diabetes, and this holds true in children as well as adults. It is
estimated that the chance to develop diabetes doubles for every 20% increase
over desirable body weight.
Diabetes mellitus, describes a collection of
metabolic diseases in which the person has high blood glucose (blood sugar),
either because insulin production is insufficient, or because the body's cells
do not react correctly to insulin, or both. Patients with high blood sugar will
usually experience polyuria (frequent urination), they will become increasingly
thirsty (polydipsia) and hungry (polyphagia).
All
types of diabetes are treatable. Diabetes type 1 lasts a lifetime, there is no
known cure. Type 2 usually lasts a lifetime, however, thousands of people have
managed to get rid of their symptoms without medication and also within the
shortest period of time by learning and applying the secrets in HERE
Researchers from the Mayo Clinic Arizona in
Scottsdale showed that gastric bypass surgery can reverse type 2 diabetes in a
high amount of patients. They added that within three to five years the disease
recurs in roughly 23% of them. Yessica Ramos, MD., said "The reappearance
rate was primarily influenced by a longstanding history of Type 2 diabetes
before the surgery. This suggests that early surgical intervention in the
obese, diabetic inhabitants will improve the permanence of remission of Type 2
diabetes.
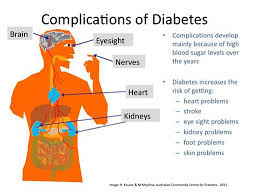
If diabetes is not adequately controlled the patient
has a significantly higher risk of developing complications such as :
Eye complications - glaucoma, cataracts, diabetic retinopathy, and some
others.
Foot complications - neuropathy,
ulcers, and occasionally gangrene which may entail that the foot be amputated
Skin complications - people
with diabetes are more vulnerable to skin infections and skin disorders
Heart problems - such
as ischemic heart disease, when the blood supply to the heart muscle is
diminished
Hypertension -
familiar
in people with diabetes, which can raise the risk of kidney disease, eye
problems, heart attack and stroke
Mental health - unrestrained
diabetes raises the risk of suffering from depression, nervousness and some
other mental disorders
Hearing loss -
diabetes
patients have a higher danger of developing hearing problems
Gum disease -
there
is a much higher occurrence of gum disease among diabetes patients
Gastroparesis - the
muscles of the stomach stop working correctly
Ketoacidosis -
a
combination of ketosis and acidosis; gathering of ketone bodies and acidity in
the blood.
Neuropathy -
diabetic
neuropathy is a type of nerve damage which can lead to numerous different
problems.
HHNS (Hyperosmolar Hyperglycemic Nonketotic Syndrome) - blood glucose levels shoot up too
high, and there are no ketones present in the blood or urine. It is an
emergency condition.
Nephropathy -
uncontrolled
blood pressure can lead to kidney disease
PAD (peripheral arterial disease) - symptoms may contain pain in the leg,
tingling and at times problems walking correctly
Stroke - if blood
pressure, cholesterol levels, and blood glucose levels are not controlled, the
risk of stroke increases
drastically
Erectile dysfunction - male
impotence.
Infections -
people
with badly controlled diabetes are much more susceptible to infections
Healing of wounds - cuts
and lesions take much longer to heal
The only way to solve your diabetes problems within the shortest period of time is HERE AGAIN
The only way to solve your diabetes problems within the shortest period of time is HERE AGAIN